- Also from Pulse
- Pulse NEWS
- Pulse CPD
- Pulse JOBS
- Pulse EVENTS
Primary Care Networks are being encouraged to employ Health and wellbeing coaches under the Additional Roles Reimbursement Scheme. GP partner and PCN co-clinical director Dr Rupa Joshi explains what this relatively new role involves, how it can benefit your practice and how to go about employing the right person for the role.
Lifestyle medicine approaches and patient education form a large basis of consultations within general practice.1
However, with only 10-minute appointments, it can be difficult to motivate patients to fully encompass these approaches into their day-to-day lives.
Employing a health and wellbeing coach can be the key to preventative medicine, self-care promotion and, in time, reducing general practice appointments.
At this time, during the Covid-19 pandemic, patients are taking a closer look at self-care and wellbeing and how to best keep themselves healthy and free from disease, especially with media attention on the role of obesity in the prognosis of COVID-19.
This is an excellent time and opportunity to approach these patients and offer them advice on changing their lifestyle for health promotion and to reduce the disease burden on practices and the NHS. 2
Health Education England (HEE) defines health coaching as follows: ‘Health coaching is a partnership between health and care practitioners and people. It guides and prompts people to change their behaviour, so they can make healthcare choices based on what matters to them.’3
Health coaching also supports patients to become more proactive in their health and care. NHS England’s Universal Personalised Care framework includes the following definition of health coaching, as part of supported self-management approaches: ‘Helping people gain and use the knowledge, skills and confidence to become active participants in their care so that they can reach their self-identified health and wellbeing goals.’4
A health and wellbeing coach supports proactive holistic patient care and helps to motivate patients to sustain lifestyle changes. A health coach can work across different sites, carrying out consultations face to face or remotely via video or telephone consultation. The health coach will take referrals from the GP practice and, based on the patient’s needs, provide 1:1 sessions offering individual tailored support, or group lifestyle education sessions offering clinician-led discussions and peer support. They can also be involved in multidisciplinary team (MDT) group consultations with the patient. It is vital that there is a system to exclude red flags prior to a patient being referred to the health coach.
Areas of general practice where health and wellbeing coaches can support practices and potentially alleviate GP workload include:
Clinicians and staff at your Primary Care Network (PCN) should be involved in shaping the particular service your health and wellbeing coaches provides. The service should be aligned within the system and other clinical pathways such that it fits in with other supported self-management interventions that may exist locally.
The role can tie in with the overall strategy of the practice or PCN in improving the health of their residents, those with long term conditions, frequent attenders, tackling health inequalities or using population health management data to guide the inclusion criteria for referral.
The health coach could be expected to deliver:
See box below for further information on each of these.
It is essential to find someone who you feel would fit in well into your team and have experience of working with the challenges of your particular population. A health and wellbeing coach with life experience, personal characteristics of active listening and empathy, and the ability to adapt their coaching skills to the individual would be ideal. PCNs may be able to hire someone who is already trained in coaching, or could employ someone with life experience and then provide training. Many training hubs have organised or are in the process of organising this training on behalf of PCNs.
There are professional coaching bodies such as the International Coach Federation (ICF), European Mentoring Coaching Council (EMCC), Association of Coaching (AoC) and UK Health Coaches Association, all of which require members to adhere to codes of conduct and ethics with associated complaints procedures.
Recommended training for the post is for at least four full days run by accredited bodies and ongoing reflective supervision is advised.5
The costs to a PCN of employing a health and wellbeing coach are reimbursed by the ARRS, with the maximum for the salary set at Band 5 of NHS Agenda for Change.6
Initial training is provided on the job and would be paid through an upfront investment, which could be claimed under the PCN development fund. There may also be the opportunity for train the trainer programmes and Health and Wellbeing Coaching Champions across localities and PCNs.
The role requires a clinical supervisor to provide support and mentorship. Each PCN would need to put in place a lead clinician and admin manager who would be allocated to supervise and support the health coach and aid quality improvement, audit data collections and evaluation to ensure good outcomes, and also ensure that the health and wellbeing Coach is well supported in understanding NHS requirements and that no red flags are missed. The supervision costs could also be claimed under the PCN development fund envelope.
Health coaching has a considerable evidence base. Most of the initial development of health coaching was undertaken in other countries, but there have subsequently been several well evaluated pilots of health coaching in the UK showing positive outcomes for both health and social care professionals and people.
A high-level overview of available evidence is presented in Annex D of NHS England’s Health Coaching Implementation and Quality Summary Guide: Technical Annexes.7 This reports outcomes of health coaching as follows:
More specifically, in Horsham and east Sussex direct monitoring of 372 patients who availed of the service over a two and a half year period showed a reduction in non-elective admissions and Accident and Emergency attendances, as well as significant increases in patient activation measures and positive impact on long-term behaviour change leading to reductions in system use.
In our experience, contacts with the health coach have been greatly valued by patients. We have observed emails of thanks sent to the practice following appointments. There has been praise of using a personalised care approach and giving patients time and space, and giving advice empowering patient to be able to cope with their long term conditions.
There is the possibility that the health coach could be referred very complex patients who may need more time per session, and require more than their allocated number of sessions. Such patients may have been living with multiple co-morbidities and find it difficult to be motivated. There is also the possibility of building dependence.
As with other roles appointed via the ARRS, another potential challenge is how to ensure parity of access and value to member practices.
At our PCN for the first three months after the new staff member starts, their position and performance are discussed at the NOG meeting on a monthly basis, thereafter on a three-monthly basis for the first year. This is to ensure that we are keeping track of their progress, and gives practices a chance to input on any major changes required in the role. It will also allow feedback to the NOG group regarding their quality improvement work as a team.
Records should be kept of referrals and follow-ups per practice. If there is a concern regarding their allocation between practices, this can be addressed and resolved at these scheduled meetings.
Case Study: Male patient with sleep apnoea.
This gentleman was triaged for feeling ‘tired all the time’ and on closer questioning, his symptoms sounded like sleep apnoea. He was also taking medication for hypertension. Options for management were discussed, and the patient was keen to see the health and wellbeing coach for lifestyle and weight loss advice.
At his initial health coaching consultation he was given recommendations for diet and for reducing his level of caffeine.
At his 4-week follow-up appointment, he had lost half a stone in weight and reported to be feeling 50% more energetic. He has not consulted the GP for his concern since seeing the health coach.
Patient testimonies
‘Fascinating, informative, thought provoking and good to reflect on’
‘I have enjoyed listening to the presentation and found the way of looking at lifestyle so much easier to understand’
‘Lovely and clear, well presented message’
‘Thank you for this very informative session. I will follow this up for sure!’
Dr Rupa Joshi is managing partner at Woodley centre surgery, co-clinical director for Wokingham North PCN, faculty GP for Time for Care and South-Eastern region representative for the NHS Confederation PCN board
References
1. Egger G, Sagner M, Meldrum et al. A structure for Lifestyle medicine. In Lifestyle Medicine: 47-63. London: Elsevier Academic Press (2017)
2. DiClemente C and Velasquez M. Motivational interviewing and the stages of change. In Motivational interviewing: Preparing people for change (2nd Edition): 201-216 New York: Guilford Press (2002)
3. Health Education England. What is Health Coaching? https://www.hee.nhs.uk/our-work/health-coaching
4. NHS England. Tools to implement supported self-management.
5. NHS England. Universal personalised care: Implementing the comprehensive model.
6. NHS Employers. Agenda for Change Pay scales
7. NHS England. Health Coaching Implementation and Quality Summary Guide: Technical Annexes. Annex D: Evidence
Lifestyle group education sessions
These can be done online using remote conferencing software such as Microsoft Teams, with groups invited from each PCN member practice. Topics may include:
– Healthy eating for a healthy lifestyle
– Diabetes and Lifestyle
– Understanding the Function of Sleep for Health and Well-being
– Want to exercise but don’t have the time? (Understanding the Function of Exercise/Movement for Health and Well-being.)
– Understanding the Impact of Stress on our Health and Some Stress Relieving Techniques.
– Using Lifestyle to improve your mental health
– Menopause – how to improve your symptoms using lifestyle techniques
Group consultations/ Virtual Group Consultations
The health coach can play a key role in facilitating and providing clinical input as part of the multidisciplinary team (MDT) in the delivering of group consultations, both face to face and remotely (virtual group consultations). The MDT can include social prescribing link workers, mental health therapists and voluntary sector workers and community colleagues such as the health visiting team, and secondary care colleagues such as pain consultant or physiotherapists. Patient cohorts may include:
– Asthma
– Anxiety
– Children’s Mental Health
– Postnatal care
– Chronic pain
– Fibromyalgia
– Diabetes
– Minor illness in under 5s
– Shielding Q&A
– Carers
1:1 Sessions
The health coach will also deliver ‘1:1 sessions’ to support an individual’s need for lifestyle changes with general tips and motivational tools.
The main interventions they use are based on five lifestyle pillars of health and wellbeing (see Figure 1).
The sessions can be provided online via conference software or by telephone, or face to face when safe to do so.
New patients have an initial 30-minute consultation followed by up to two 15-minute sessions. Each patient is given a lifestyle questionnaire to complete and return one week before their initial consultation. This collates patient goals, their general state of health, nutrition and lifestyle and saves time during the consultation so that the health coach can suggest some tools and build an action plan.
After each consultation the coach has to formulate a joint personalized action plan to forward along with relevant information leaflets to the patient.
Suitable patients for referral include those with:
– Diabetes
– Hypertension/ CHD
– Weight management
– Poor nutrition/ diet
– Anxiety and Depression
– Stress
– Sleeping problems
– Chronic fatigue
– Coping with long term conditions
– Frequent Attenders
– Patients with health inequalities
A health and wellbeing coach could also run sessions for all staff across the PCN on lifestyle and self-care. He/she could also organise health and wellbeing campaigns via posters, website blogs and posts for social media for the practice/ PCN.
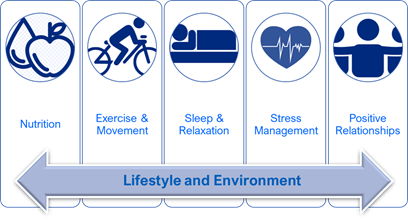
Figure 1 – The main lifestyle pillars of health and wellbeing
Or, please register for a free trial to access all of the guides and unlock all features.